Biomarkers & Immunotherapy
Cancer rates are climbing fast, and by 2050, more than 35 million people worldwide are expected to be affected(1) That makes the search for better, more effective treatments more important than ever. From 1990 to 2021, the global burden of melanoma on healthcare systems has risen. In that time, the number of individuals aged 65 and older diagnosed with skin cancer reached nearly 4.42 million(2) Research models also project a sharp rise (more than a 140 % increase) in the rate of newly diagnosed basal cell carcinoma cases(2).
Such findings emphasize a pressing need for targeted prevention strategies to effectively tackle this growing issue.
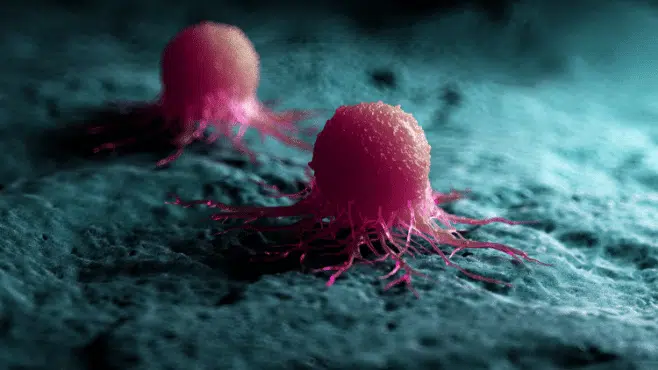
Over the last decade, oncology research has shifted its attention towards developing personalized treatments, designed to target cancerous cells. Targeted immunotherapies are improving patient survival rates, increasing the safety of treatments, and improving the overall quality of life of cancer patients(3).
A big part of this progress comes down to biomarkers. In melanoma in particular, biomarkers are helping guide treatment choices and tailor therapies to match not just the tumor, but the patient’s unique immune system. That level of personalization can improve results and reduce the risk of unnecessary side effects.
Apart from BRAF V600E mutations, some of the most important biomarkers in melanoma right now include PD-L1 expression, tumor mutational burden (TMB), and tumor-infiltrating lymphocytes (TILs). There’s also a growing focus on combining multiple markers, looking at genetic, immune, and molecular data together, to get a fuller picture and make even more accurate predictions(4).
Challenges with Immunotherapy Treatment of Melanoma: A Need for More Reliable Biomarker Analysis Strategies
Although the introduction of immunotherapy has resulted in significant advancements in the treatment of melanoma, patient responses are still highly variable, highlighting an existing need for more reliable biomarker analysis(4).
The reality is that most patients either don’t respond to immunotherapy at all or relapse after an initial response. This can be driven by tumor-intrinsic changes, an immunosuppressive tumor microenvironment, or simply by enrolling the wrong patients in clinical trials. For trial sponsors, this creates a challenge: how do you design biomarker strategies that can keep up with the constantly shifting biology of resistance?
Too often, trials fail to properly monitor key factors like loss of antigen presentation, T cell exclusion, microenvironmental suppression, or the tumor’s adaptive evolution. As a result, resistance (both primary and secondary) to checkpoint inhibitors like PD-1/PD-L1 and CTLA-4 remains high. This translates into poor durability of treatment,elevated failure rates and reduced progression-free survival(5,6).
Difficulties also arise when integrating and operationalizing multimodal biomarkers (next-generation sequencing (NGS), PD L1 and immune IHC, TMB, MSI, TIL density, cytokines, ctDNA, microbiome) across global sites with consistent quality, turnaround, and regulatory-grade data.
Understandably, sponsors are hesitant to pour resources into a melanoma immunotherapy program if the biomarker strategy is mis-specified, due to factors such as wrong cut-offs, wrong assays, wrong sampling timepoints, and, as a result, it can make it nearly impossible to explain why some patients don’t respond, or to find a way to help them. With Cerba Research, however, you could have the benefit of a scientific consultation on biomarker strategy, sampling timepoint, and cut-offs to assess the response/non-response.
There’s also growing caution around lab partners. A lab might be great at running a specific technology but lack the ability to support integrated biomarker strategies, rescue assays for non-responders, or adaptive trial designs. This can delay first patient in (FPI) timelines and stall key regulatory conversations. Cerba Research helps ease customer concerns by offering a lab partnership that supports an integrated biomarker strategy, while also being equipped to rescue studies or assays for non-responders or adapt to adaptive trial designs. This can delay first patient in (FPI) timelines and stall key regulatory conversations. Cerba Research helps ease customer concerns by offering a lab partnership that supports an integrated biomarker strategy, while also being equipped to rescue studies or assays for non-responders or adapt to adaptive trial designs
Cerba Research’s State-of-the-Art Biomarker Guided Strategies
At Cerba Research, we specialize in laboratory services that support biomarker discovery and assessment, offering expertise in immunohistochemistry (IHC), flow cytometry (FCM), genetics/genomics, and immunoassays.
From the earliest stages of a project, our scientific team works closely with sponsors to design fit-for-purpose assays that align with each study’s specific goals.
A key area of focus is helping our sponsors overcome melanoma immunotherapy resistance by building biomarker strategies that capture antigen presentation loss, T cell dysfunction, and tumor microenvironment changes through coordinated IHC, NGS, flow/spectral flow, and liquid biopsy broad panel assays (ctDNA).
Our multi-platform biomarker-guided trial designs (e.g., PD-L1 IHC (clones 22C3, SP142, SP263, multiplexed), TMB/NGS panels, TIL and T cell phenotyping, ctDNA broad panel assays for early relapse/response) and consultative Centre of Excellence help to ensure reliable results that overcome the challenges described above.
Cerba Research supports the advancement of all-important personalized immunotherapy in melanoma by consistently linking baseline and on-treatment biomarkers, such as PD-L1, TMB, TIL signatures, gene expression, and ctDNA panels, to smarter patient selection, dosing strategies, and treatment decisions. This includes biomarker-driven strategies for both checkpoint and TIL-based therapies, with the ability to track resistance patterns and adjust treatment accordingly.
Our technology platforms and in-house expertise span the full spectrum of melanoma testing, from flow cytometry and histopathology to molecular diagnostics and NGS.
Thanks to our central laboratory infrastructure, we’re able to streamline study setup, often getting trials up and running in as little as 6 to 8 weeks, depending on complexity. We also offer comprehensive bioanalytical services across preclinical (GLP and non-GLP) and clinical phases, covering primary, secondary, and exploratory endpoints.
As a leading provider of specialty laboratory services, Cerba Research combines scientific depth with the reach of a global central lab network. We deliver high-quality research across key international locations, including New York, Ghent, Taipei, Sydney, Paris, Shanghai, Rotterdam, Rijswijk, and Montreal.
Invaluable Innovation in Biomarker-driven Immunotherapies at Cerba Research
Our highly qualified scientists offer invaluable insights into the latest biomarkers, assays, and testing approaches. With a mix of hands-on experience and access to cutting-edge technology, we help sponsors tackle challenging issues across all phases of melanoma immunotherapy research.
At Cerba Research, we are the laboratory partner that you can trust to design and operationalize your biomarker-driven immunotherapy trials in melanoma therapeutic research (including checkpoint inhibitors, TILs, combinations) through integrated PK/PD, IHC, NGS, flow/spectral flow, and central lab platforms.
We are proud to provide innovative specialty lab services (IHC, FCM, genetics/genomics and immunoassays) dedicated to biomarker assessment and discovery to our diverse sponsors – pharmaceutical, biotechnology, medical device, government, public health, and CRO organizations.
Find out more about how Cerba Research can effectively guide your biomarker analysis for immunotherapy research in melanoma.